Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by airflow obstruction that makes breathing difficult. It includes conditions such as emphysema and chronic bronchitis. The primary causes of COPD are long-term exposure to harmful particles or gases, most commonly from smoking. However, environmental pollutants, genetic factors, and respiratory infections can also contribute to the development and progression of the disease.
Although COPD is a chronic condition with no known cure, lifestyle changes can play a pivotal role in improving the quality of life, slowing disease progression, and reducing symptoms. Through tailored lifestyle adjustments, COPD patients can experience better lung function, reduced flare-ups, and a more active, fulfilling life. In this article, we will explore how lifestyle changes can improve COPD management, covering diet, physical activity, smoking cessation, managing stress, and other behavioral modifications that can lead to substantial improvements in health outcomes.
Key Takeaways
- Smoking cessation is the most effective way to slow the progression of COPD.
- A balanced diet with adequate protein, fruits, vegetables, and limited processed foods supports lung health.
- Physical activity is essential for strengthening the lungs and improving stamina.
- Mental health management is critical in reducing stress, which can worsen COPD symptoms.
- Regular medical check-ups ensure that the disease is being properly managed and that treatment plans are adjusted as needed.
Introduction to COPD and Its Impact
Chronic Obstructive Pulmonary Disease (COPD) is a leading cause of morbidity and mortality worldwide. According to the World Health Organization (WHO), COPD affects over 250 million people globally, and it is projected to become the third leading cause of death by 2030. COPD can cause severe damage to the lungs and result in symptoms such as chronic cough, shortness of breath, wheezing, and frequent respiratory infections.
Although COPD is a progressive disease, lifestyle modifications can make a significant difference in managing symptoms and improving the overall quality of life. Since COPD is often diagnosed at an advanced stage, making changes early can help slow disease progression and improve outcomes.
The Role of Lifestyle Changes in COPD Management
Managing COPD is a multi-faceted approach, where the integration of various lifestyle changes can have a profound impact on both short-term symptom relief and long-term disease management. While medical treatment, such as medications and oxygen therapy, is essential, adopting healthy behaviors is equally important. These lifestyle changes not only help manage symptoms but also contribute to overall well-being, improve lung function, reduce the frequency of exacerbations, and enhance the ability to perform daily activities.
The primary lifestyle changes that improve COPD management include:
- Smoking cessation
- Dietary improvements
- Physical activity and exercise
- Stress and anxiety management
- Adequate rest and sleep
- Hydration
- Minimizing exposure to pollutants
Each of these areas plays a vital role in enhancing lung function, reducing symptoms, and improving the overall quality of life for COPD patients.
Smoking Cessation: The First Step in COPD Management

The most important lifestyle change for COPD patients is quitting smoking. Smoking is the leading cause of COPD, and even in non-smokers, secondhand smoke can contribute to the development of the disease. Smoking damages the airways and accelerates the decline in lung function. Quitting smoking is the most effective way to slow the progression of COPD and improve lung health.
- Benefits of Smoking Cessation:
- Reduced inflammation: Smoking causes inflammation in the lungs, making the airways more susceptible to damage. Quitting smoking reduces this inflammation, which in turn helps to preserve lung function.
- Improved lung function: After quitting, the lungs begin to heal, and airflow can improve, especially in the earlier stages of COPD.
- Reduced risk of exacerbations: Smoking increases the likelihood of respiratory infections and flare-ups. By quitting, patients reduce their risk of these complications.
There are many resources available to help smokers quit, including nicotine replacement therapies (NRT), prescription medications, counseling, and support groups.
Nutritional Adjustments to Support Lung Health
A well-balanced diet is crucial for maintaining good overall health, particularly for those with COPD. Nutritional choices can directly impact lung function, energy levels, and the ability to fight infections. COPD patients often have higher energy needs, especially if they experience frequent flare-ups.
- Foods to Include:
- Fruits and vegetables: Rich in antioxidants, these foods help combat oxidative stress and inflammation, which are common in COPD patients.
- Lean proteins: Protein is essential for repairing lung tissue and maintaining muscle mass, which can deteriorate due to the increased effort of breathing.
- Whole grains: Complex carbohydrates provide energy without contributing to inflammation.
- Foods to Avoid:
- Excessive sodium: High sodium levels can lead to fluid retention, worsening symptoms like shortness of breath and swelling.
- Fried and fatty foods: These foods can increase inflammation and make breathing more difficult.
- Dairy products: Some COPD patients may find that dairy increases mucus production, so reducing dairy intake may be beneficial.
Consulting with a dietitian or nutritionist who understands the specific needs of COPD patients can help tailor a diet that supports lung health and overall well-being.
Physical Activity and Exercise: Strengthening the Lungs
Physical activity is one of the most effective ways to improve lung function and overall health for COPD patients. While COPD may make it difficult to exercise, regular physical activity can significantly enhance breathing capacity, reduce shortness of breath, and increase stamina.
- Benefits of Exercise for COPD:
- Improved lung capacity: Cardiovascular exercises such as walking, swimming, or cycling can improve circulation and oxygen uptake, making breathing easier.
- Strengthening muscles: COPD patients often experience muscle weakness, especially in the legs. Strength training exercises can help preserve muscle mass and improve mobility.
- Reduced fatigue: Regular exercise improves energy levels and reduces feelings of fatigue, which is a common issue for COPD patients.
- Enhanced mental health: Physical activity helps alleviate anxiety and depression, common in COPD patients due to the chronic nature of the disease.
Exercise should be tailored to each individual’s capabilities. A pulmonary rehabilitation program is an excellent way to safely incorporate exercise under medical supervision.
Managing Stress and Mental Health for Better Respiratory Health

Chronic stress, anxiety, and depression can have a negative impact on COPD management. Stress can trigger flare-ups, worsen symptoms, and interfere with medication adherence. Mental health is intrinsically linked to physical health, especially for those managing a chronic disease like COPD.
- Strategies to Manage Stress:
- Breathing exercises: Techniques such as pursed-lip breathing can help reduce stress and improve airflow, making it easier to breathe.
- Mindfulness and meditation: These practices reduce anxiety and stress, improve focus, and help with relaxation.
- Cognitive behavioral therapy (CBT): This therapeutic approach helps patients manage negative thoughts and emotional responses, which can alleviate anxiety and depression.
- Social Support: Staying connected with family, friends, or support groups can help combat feelings of isolation, a common concern for people with chronic diseases.
Sleep Hygiene: The Importance of Rest for COPD Patients
COPD patients often struggle with sleep disturbances due to shortness of breath, coughing, or other symptoms. Poor sleep quality can contribute to fatigue, cognitive impairment, and increased risk of complications.
- Improving Sleep Quality:
- Elevating the head: Using pillows or a recliner to elevate the head while sleeping can make breathing easier.
- Avoiding large meals before bedtime: Large meals can exacerbate acid reflux, which can worsen symptoms during the night.
- Establishing a regular sleep schedule: Going to bed and waking up at the same time every day helps regulate the body’s circadian rhythm.
- Using supplemental oxygen at night: For patients with advanced COPD, using supplemental oxygen during sleep may improve sleep quality.
Staying Hydrated: How Fluids Benefit Lung Health
Proper hydration is essential for lung health, especially for COPD patients. Dehydration can lead to thicker mucus in the airways, making it more difficult to clear the lungs and causing further respiratory issues.
- Hydration Benefits:
- Thins mucus: Drinking water helps thin the mucus in the lungs, making it easier to expel.
- Prevents fatigue: Staying hydrated helps maintain energy levels and overall vitality.
COPD patients should aim for adequate fluid intake, usually 6-8 cups of water per day, unless otherwise advised by a doctor due to other medical conditions (e.g., heart disease).
Pollution and Air Quality Control: Reducing Lung Irritants
Exposure to environmental pollutants, allergens, and irritants can worsen COPD symptoms. Managing indoor and outdoor air quality is crucial in COPD management.
- Pollution Control Tips:
- Air purifiers: Use air purifiers at home to remove allergens and pollutants from the air.
- Avoiding outdoor activities during high pollution levels: Check air quality indexes and limit outdoor exposure on days with high pollution.
- Ventilating your home: Keep windows open or use exhaust fans to improve airflow and reduce indoor pollution.
Preventing Infections: Vaccinations and Hygiene Measures
COPD patients are more susceptible to respiratory infections, which can lead to exacerbations and further lung damage. Preventing infections through vaccinations and good hygiene practices is essential.
- Vaccinations:
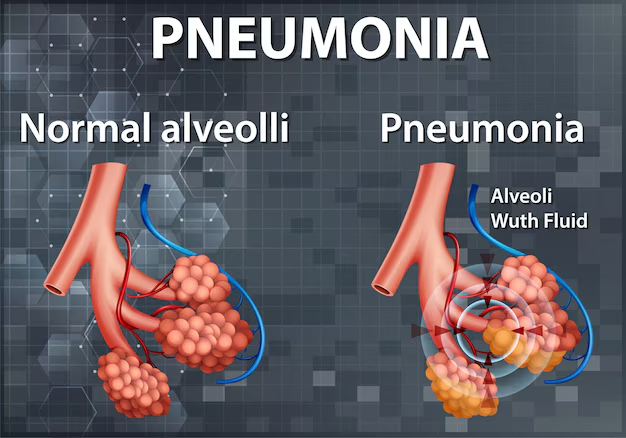
- Flu shot: Annual flu vaccination is recommended for COPD patients to prevent the flu.
- Pneumonia vaccine: Pneumococcal vaccination helps prevent pneumonia, a serious complication for COPD patients.
- COVID-19 vaccine: Given the respiratory complications of COVID-19, vaccination is crucial for individuals with COPD.
- Hygiene Practices:
- Regular handwashing: To reduce the spread of infections.
- Avoiding close contact with sick individuals: Minimize exposure to respiratory infections, especially during cold and flu season.
Adhering to Treatment Plans and Regular Check-ups
It is important for COPD patients to adhere to their prescribed treatment plans, including medications, oxygen therapy, and other interventions. Regular check-ups with healthcare providers help monitor disease progression and adjust treatment as necessary.
The Importance of Self-Monitoring and Tracking Symptoms

For individuals with COPD, self-monitoring is essential to detect any changes in symptoms and seek timely medical intervention. Regularly tracking symptoms such as breathlessness, coughing, sputum production, or fatigue can help you understand your condition better and communicate effectively with your healthcare provider.
Why is Self-Monitoring Important?
- Early Intervention: By noticing a change in symptoms early, you can take measures to prevent a full-blown exacerbation.
- Empowerment: Self-monitoring gives you a sense of control over your health and enables proactive management.
- Better Communication: When you track your symptoms, your healthcare provider can make better-informed decisions regarding treatment.
Some useful tools for monitoring include peak flow meters, which measure airflow in your lungs, and pulse oximeters, which measure blood oxygen levels. Keeping a symptom diary or using an app to track your progress can also be helpful.
The Role of Medications and Inhalers in Lifestyle Management
While lifestyle changes are crucial for COPD management, medications play an equally significant role in controlling symptoms. Medications like inhalers, bronchodilators, corticosteroids, and other drugs are vital for managing COPD effectively.
Understanding the Role of Inhalers Inhalers deliver medications directly to the lungs, helping to reduce inflammation and open up the airways. Bronchodilators, for instance, help widen the airways, making breathing easier. Steroid inhalers reduce inflammation in the lungs, preventing exacerbations.
Other Medications for COPD
- Long-acting bronchodilators: These medications help maintain airflow for a longer duration and prevent sudden shortness of breath.
- Steroids: Inhaled corticosteroids are used to reduce inflammation in the airways, helping to prevent flare-ups.
- Antibiotics: For some patients with chronic bacterial infections, antibiotics may be prescribed to prevent recurrent infections.
- Phosphodiesterase-4 inhibitors: These can help decrease inflammation and relax the airways.
Adherence to your prescribed medication regimen is crucial. It’s important to work with your healthcare provider to adjust medications as needed.
Travel Considerations for COPD Patients
Traveling can be challenging for COPD patients, especially when it involves long flights or exposure to different environmental conditions. However, with proper planning, traveling can still be enjoyable and safe.
Travel Tips for COPD Patients:
- Plan Ahead: Before traveling, discuss your plans with your healthcare provider to ensure you’re prepared for any possible complications.
- Bring Extra Medication: Carry enough medication for the entire trip, plus extra in case of delays or unforeseen circumstances.
- Travel Insurance: Look into travel insurance that covers pre-existing conditions like COPD. This can provide peace of mind in case you need medical attention during your trip.
- Oxygen Needs: If you require supplemental oxygen, check with the airline or transportation provider about their oxygen policies. Some airlines provide oxygen on board, but arrangements must be made in advance.
- Stay Hydrated: Air travel can cause dehydration, which may exacerbate breathing difficulties. Be sure to drink plenty of fluids and avoid alcohol and caffeine.
By being proactive about managing your COPD during travel, you can ensure a safe and comfortable experience.
The Importance of Support Networks
Living with COPD can be isolating, both physically and emotionally. Having a strong support network of family, friends, and healthcare providers is essential for coping with the daily challenges of managing a chronic illness.
How Support Networks Help:
- Emotional Support: A strong support system helps reduce feelings of loneliness and anxiety. It can also provide encouragement when sticking to a treatment plan or making lifestyle changes.
- Physical Assistance: Family members or caregivers can help with tasks that may be difficult due to fatigue or breathlessness, such as preparing meals or attending doctor appointments.
- Educational Support: Support groups, both in-person and online, provide valuable resources and information for managing COPD. Sharing experiences with others facing similar challenges can offer both emotional and practical benefits.
Joining a COPD support group can be incredibly helpful in learning new coping strategies, managing stress, and building lasting relationships with others who understand the disease. Additionally, some healthcare providers offer group therapy or individual counseling to address mental health concerns.
Understanding the Stages of COPD and Tailoring Management
COPD progresses through different stages, from mild to very severe. The severity of the disease is determined by how much airflow is limited and the frequency of exacerbations. Understanding the stages of COPD can help guide treatment and lifestyle decisions.
The Stages of COPD:
- Mild (Stage 1): Early stages of COPD may not show noticeable symptoms. There is slight airflow limitation, but people may not be aware of it.
- Moderate (Stage 2): Symptoms such as shortness of breath and cough become more noticeable. Exacerbations may occur, requiring treatment.
- Severe (Stage 3): Symptoms become more persistent and limiting. Frequent flare-ups can cause major disruptions to daily activities.
- Very Severe (Stage 4): At this stage, COPD can cause significant respiratory distress, and lung function is severely impaired. Oxygen therapy and other interventions are often required.
COPD management should be tailored to the stage of the disease. Early-stage COPD may benefit more from lifestyle changes, while later stages require a combination of medication, therapy, and support.
Also Read: What Is Care Coordination? A Comprehensive Guide
Conclusion
Lifestyle changes play a pivotal role in managing COPD and improving overall quality of life. While COPD is a chronic and progressive disease, adopting healthy habits such as smoking cessation, improving diet, exercising regularly, managing stress, and improving sleep hygiene can significantly reduce symptoms, slow disease progression, and enhance lung function. By incorporating these changes into daily life, COPD patients can lead healthier, more active lives and reduce the frequency of exacerbations.
Managing Chronic Obstructive Pulmonary Disease (COPD) effectively requires a multifaceted approach that combines medication, lifestyle changes, and emotional support. Lifestyle modifications such as smoking cessation, maintaining a healthy diet, staying active, and managing stress can significantly improve symptoms and quality of life. By staying proactive and committed to their health, COPD patients can experience fewer flare-ups, better lung function, and a more fulfilling life.
The key to managing COPD is to make small, consistent changes and work with your healthcare provider to create a personalized management plan. Although COPD is a chronic condition, effective management allows individuals to live longer, healthier lives and maintain a good quality of life.
FAQs
How can exercise benefit COPD patients?
Exercise improves lung capacity, reduces shortness of breath, and enhances overall strength.
Is it possible to reverse COPD?
COPD is a progressive disease, but early interventions and lifestyle changes can slow its progression.
Can dietary changes help manage COPD symptoms?
Yes, a healthy diet rich in antioxidants and low in processed foods can reduce inflammation and support lung health.
What is the best way to stop smoking?
Nicotine replacement therapy, counseling, and support groups can help people quit smoking.
How important is sleep for COPD patients?
Adequate sleep is essential to manage fatigue, reduce inflammation, and improve overall health.
How can I avoid flare-ups of COPD?
Minimize exposure to pollutants, follow your treatment plan, get vaccinated, and manage stress.
Should I consult a pulmonologist for COPD management?
Yes, pulmonologists specialize in lung diseases and can provide a tailored treatment plan for managing COPD.

