Mental health is a crucial aspect of overall well-being, yet it often remains overlooked or under-treated. As society becomes more aware of mental health conditions and their impact, it’s essential to understand how a structured, comprehensive mental health care pathway can help individuals receive the best care throughout their journey—from diagnosis to recovery. A comprehensive mental health care pathway is a holistic approach that incorporates various stages of care, from early intervention to rehabilitation and long-term management.
This article explores the concept of a comprehensive mental health care pathway, examining each phase of the process, the importance of a multidisciplinary approach, and how it helps individuals regain their mental health and live fulfilling lives. We will also address frequently asked questions (FAQs) to clarify common misconceptions about the mental health journey and provide guidance on how to navigate it effectively.
Key Takeaways
- Mental health care is a journey: From diagnosis to recovery, it involves various stages, including early intervention, treatment, crisis management, and long-term maintenance.
- Multidisciplinary care is essential: Collaboration between psychiatrists, psychologists, therapists, nurses, and other specialists ensures that the care provided is comprehensive and holistic.
- Recovery is not linear: It takes time, and individuals may experience setbacks. Long-term support, including therapy and medication, is often needed.
- Family and community support matter: A strong support system helps individuals feel understood, valued, and motivated throughout the recovery process.
- Early intervention leads to better outcomes: The earlier a mental health condition is identified and treated, the more likely it is that the individual will recover successfully and avoid long-term complications.
The Phases of a Comprehensive Mental Health Care Pathway
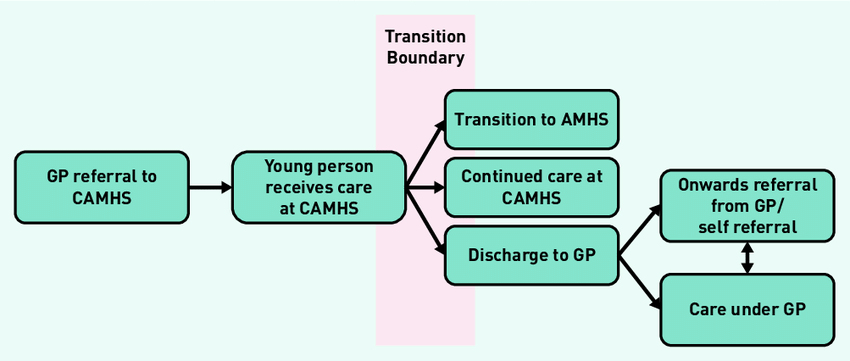
A comprehensive mental health care pathway is a step-by-step plan that ensures continuity and quality of care for individuals experiencing mental health challenges. It provides a roadmap for both patients and healthcare providers, ensuring that each phase of the care journey is handled with the appropriate level of attention and expertise. The pathway typically includes the following key stages:
1. Early Detection and Diagnosis
The first phase of the pathway focuses on the detection and diagnosis of mental health conditions. Early intervention plays a critical role in preventing the escalation of symptoms and improving long-term outcomes.
- Signs and Symptoms: Common mental health issues, such as depression, anxiety, or psychotic disorders, often go unnoticed or are misattributed to other causes. It’s important for individuals, families, and healthcare providers to recognize early signs like persistent sadness, sudden mood changes, excessive worry, or social withdrawal.
- Diagnosis Process: Accurate diagnosis is essential to ensure the right treatment plan is followed. A comprehensive assessment includes psychological evaluations, medical histories, and often, standardized diagnostic tools (such as the DSM-5 or ICD-10).
- Referral and Coordination: Following diagnosis, patients are often referred to mental health professionals such as psychiatrists, psychologists, or counselors, depending on their specific needs. This referral ensures that patients receive specialized care.
2. Treatment Planning
Once a diagnosis is made, the next step involves creating an individualized treatment plan tailored to the patient’s unique needs.
- Collaborative Approach: The treatment planning process is typically collaborative, with input from the patient, their family, and a multidisciplinary team of healthcare providers. This can include psychologists, psychiatrists, social workers, therapists, and, in some cases, occupational therapists.
- Personalized Goals: Treatment plans are based on the type and severity of the condition. They often set specific, measurable goals related to symptom reduction, functional improvement, and overall well-being.
- Evidence-Based Treatments: The treatment options may include psychotherapy (such as Cognitive Behavioral Therapy, Dialectical Behavior Therapy, or exposure therapy), medication (antidepressants, antipsychotics, anxiolytics), and lifestyle changes (diet, exercise, mindfulness techniques).
3. Acute Care and Crisis Management
In some cases, individuals may experience an acute mental health crisis that requires immediate intervention. This could be in the form of suicidal ideation, severe anxiety attacks, or a psychotic episode.
- Crisis Intervention: Immediate support may include hospitalization or outpatient care, depending on the severity of the situation. Hospitals or psychiatric units are often equipped to provide stabilization through medication, therapy, and safety monitoring.
- Short-Term Goal Setting: During this stage, the focus is on stabilizing the patient’s condition and ensuring they are safe. Short-term goals involve crisis resolution, symptom management, and providing emotional support.
4. Rehabilitation and Recovery
Recovery is a long-term process that involves building resilience, coping strategies, and restoring functioning. This phase is not linear, and many individuals will experience fluctuations in their mental health over time.
- Therapeutic Interventions: Individuals may continue with psychotherapy to build coping mechanisms and address underlying issues that contributed to their mental health condition. Rehabilitation might also include family therapy, support groups, and peer counseling to foster a sense of community and support.
- Medication Management: For many individuals with mental health conditions, ongoing medication management is necessary. Regular consultations with a psychiatrist help ensure that medications are adjusted as needed to prevent relapse or manage side effects.
- Community Integration: A key part of recovery is reintegrating into the community and workplace. Support programs, vocational training, and social skill development can help individuals rebuild their lives.
5. Long-Term Maintenance and Prevention
Once recovery is achieved, individuals enter the maintenance phase, where the goal is to prevent relapse and maintain mental health.
- Ongoing Support: Maintenance care involves regular follow-ups with healthcare providers, continuing therapy sessions, and monitoring mental health status. The goal is to address potential stressors and mitigate the risk of a relapse.
- Wellness Strategies: A strong focus on maintaining overall wellness is key to preventing future mental health crises. Regular physical exercise, good nutrition, stress management techniques (e.g., meditation, yoga), and social connections are crucial elements in maintaining mental health.
Multidisciplinary teams enhance care: The involvement of a variety of professionals—psychiatrists, therapists, social workers, nurses, and more—ensures a well-rounded approach to mental health care, addressing all aspects of an individual’s well-being.
Family and social support are integral: Support from family members, friends, and peer groups significantly impacts mental health recovery by providing emotional stability and reinforcing a sense of connection.
Individual empowerment fosters recovery: Encouraging individuals to take an active role in their treatment—whether through self-care practices, goal setting, or coping strategies—empowers them to make positive choices and regain control of their mental health.
Mental health is a lifelong journey: Even after recovery, ongoing vigilance and care are essential. People with mental health conditions may experience ups and downs throughout life, so long-term maintenance is critical for continued well-being.
Mental health education and awareness are key: Educating individuals, families, and communities about mental health conditions helps reduce stigma, encourages earlier intervention, and promotes understanding of the recovery process.
The Role of a Multidisciplinary Team in Mental Health Care
A comprehensive mental health care pathway relies heavily on the involvement of a multidisciplinary team. This team works together to address the diverse needs of the individual, ensuring that all aspects of their care are met.
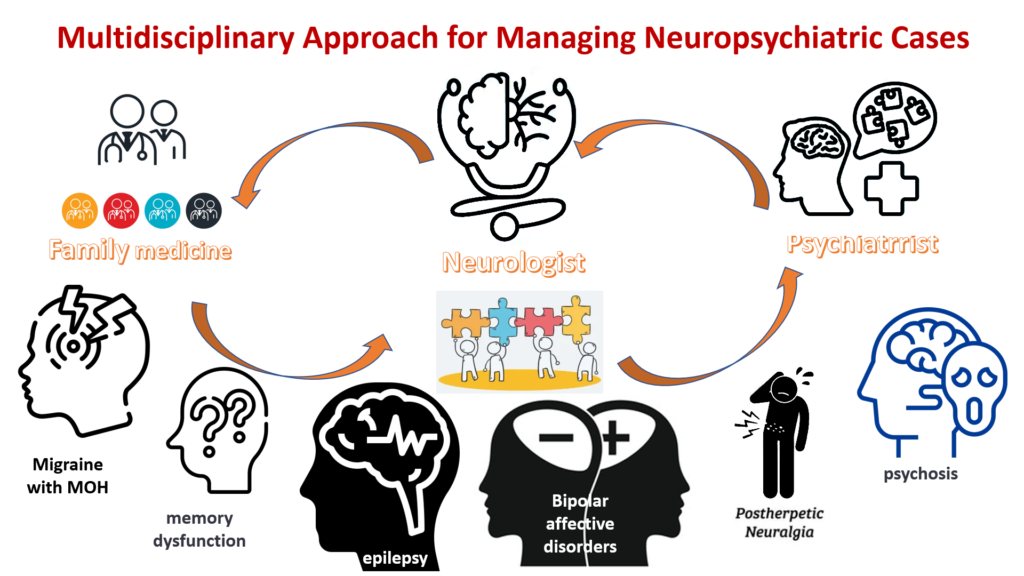
Mental health care is complex, multifaceted, and requires a broad spectrum of expertise to ensure the best outcomes for individuals. A multidisciplinary team plays an essential role in this process by offering collaborative care that addresses all aspects of an individual’s mental health. This team approach is crucial because mental health conditions often affect various dimensions of a person’s life, including emotional, psychological, physical, and social well-being.
In this article, we will explore the critical roles of each member of a multidisciplinary mental health team and how their collective efforts ensure that individuals receive comprehensive, holistic care tailored to their needs. By the end, it will be clear why such an approach is key to addressing the complexities of mental health conditions and promoting long-term recovery.
What is a Multidisciplinary Team in Mental Health Care?
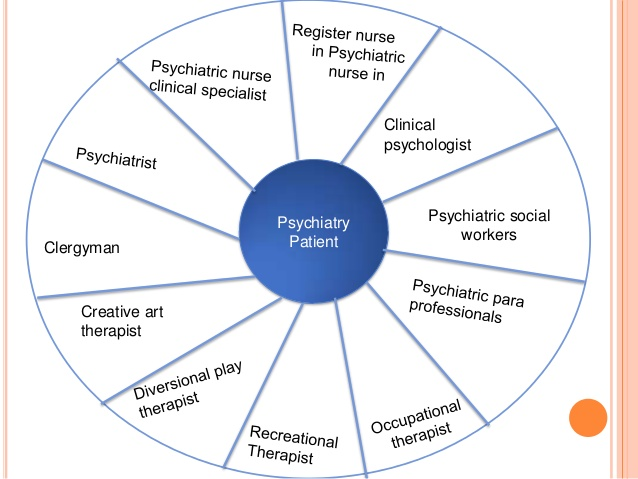
A multidisciplinary team (MDT) in mental health care consists of various professionals from different disciplines who work together to provide comprehensive, patient-centered care. The team usually includes a mix of medical, psychological, and social care providers, all of whom bring different perspectives and expertise to the care process.
In mental health care, these teams often collaborate in hospitals, outpatient clinics, rehabilitation centers, or community-based settings, where they design and implement individualized care plans, monitor progress, and make adjustments as necessary.
Key Roles in a Multidisciplinary Mental Health Team
Each member of the multidisciplinary team contributes unique skills to ensure the patient’s mental, physical, and social health are all addressed. The following are the key roles typically found in such teams:
1. Psychiatrists

Role: Psychiatrists are medical doctors who specialize in diagnosing, treating, and managing mental health disorders. They focus on understanding the biological and psychological components of a patient’s condition and are particularly skilled at addressing severe mental illnesses such as schizophrenia, bipolar disorder, and major depressive disorder.
- Responsibilities:
- Conduct comprehensive assessments and evaluations to diagnose mental health conditions.
- Prescribe medications such as antidepressants, antipsychotics, or mood stabilizers to manage symptoms.
- Monitor the effectiveness and side effects of medications, making adjustments as needed.
- Offer guidance on the overall treatment approach, coordinating with other professionals.
Psychiatrists are the key figures in managing more complex, medically sensitive aspects of mental health care and provide insights into how biological factors impact mental well-being.
2. Psychologists

Role: Psychologists, specifically clinical psychologists, focus on understanding the mental and emotional aspects of a patient’s condition. They use talk therapies and psychological interventions to help patients explore their thoughts, feelings, and behaviors.
- Responsibilities:
- Conduct psychological assessments through interviews, tests, and observations.
- Provide psychotherapy using evidence-based methods such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), or psychodynamic therapy.
- Help patients identify thought patterns and behaviors that contribute to their mental health conditions and work to change these through therapeutic techniques.
- Work with patients on building coping strategies, emotional regulation, and problem-solving skills.
Psychologists help individuals understand the underlying psychological causes of their symptoms and use therapy to alleviate emotional distress and improve coping abilities.
3. Social Workers

Role: Social workers in mental health care provide emotional support and practical assistance. They work with individuals to manage social and environmental factors affecting their mental health, such as family dynamics, housing, and financial stability.
- Responsibilities:
- Assess the social and environmental aspects that may be influencing a patient’s mental health, such as family issues or social isolation.
- Help patients access community resources, such as housing, employment, or support groups.
- Provide counseling to families and individuals to improve social support and strengthen coping mechanisms.
- Act as advocates for patients, helping them navigate healthcare systems, insurance, or legal challenges.
Social workers play a vital role in ensuring patients have the external support needed to maintain their mental health. They often bridge the gap between clinical care and real-world circumstances, making mental health care more accessible.
4. Nurses

Role: Nurses, particularly psychiatric or mental health nurses, are essential in providing day-to-day care and support to individuals experiencing mental health challenges. They offer continuous monitoring, administer medications, and assist with basic care needs.
- Responsibilities:
- Monitor patients’ physical and emotional condition, including vitals, mood, and behavioral changes.
- Administer medications as prescribed and track their effects, ensuring adherence to the treatment plan.
- Provide emotional support and a calming presence for patients during times of distress or crisis.
- Educate patients about their condition and the importance of adhering to treatment plans.
Nurses are often the most consistent caregivers, offering not only medical monitoring but also emotional support and practical guidance throughout the treatment process.
5. Occupational Therapists

Role: Occupational therapists help patients with mental health conditions regain skills necessary for daily living and functioning. These skills can include everything from managing personal hygiene to reintegrating into the workforce.
- Responsibilities:
- Assist patients in developing skills for independent living, such as managing household tasks, cooking, or personal care.
- Provide therapy aimed at improving cognitive, physical, and emotional functioning.
- Help individuals manage stress, develop time-management skills, and create routines.
- Work with patients to address difficulties in returning to work, school, or other social environments.
By helping individuals develop life skills, occupational therapists promote independence, which is crucial for long-term mental health recovery.
6. Speech and Language Therapists

Role: In some cases, speech and language therapists (SLTs) may be part of the multidisciplinary team. These professionals focus on communication disorders and cognitive difficulties, particularly those associated with mental health conditions such as brain injury, autism spectrum disorders, or neurological issues.
- Responsibilities:
- Address communication problems such as speech difficulties, comprehension issues, or social communication challenges.
- Support cognitive rehabilitation to help patients improve memory, attention, and problem-solving abilities.
- Help individuals regain the ability to articulate thoughts and interact more effectively in social settings.
SLTs can play a key role in improving a patient’s overall communication abilities, thus aiding social interactions and recovery.
7. Peer Support Workers

Role: Peer support workers are individuals who have lived experience with mental health conditions. They offer support and mentorship to others going through similar challenges, helping to reduce stigma and increase hope for recovery.
- Responsibilities:
- Share personal experiences of mental health recovery, offering encouragement and hope.
- Provide guidance on coping strategies and help individuals navigate their own recovery journey.
- Offer emotional support during times of distress, especially for those who may feel isolated in their struggles.
- Facilitate group support sessions or individual peer support meetings.
Peer support workers provide a unique perspective and foster a sense of community and shared experience that can enhance a patient’s journey to recovery.
How a Multidisciplinary Team Collaborates
The real strength of a multidisciplinary team is its ability to work together, share expertise, and ensure holistic care. Collaboration among professionals is key to creating a treatment plan that addresses all facets of a person’s mental health. For instance:
- Regular Case Meetings: The team often holds regular meetings to discuss the patient’s progress, update treatment plans, and ensure all needs are being met. Each professional provides their perspective, which creates a more complete picture of the patient’s mental health.
- Coordination of Care: One professional may be treating a particular aspect of the patient’s mental health, but this does not happen in isolation. Psychiatrists may communicate with psychologists to adjust treatment plans based on the progress of psychotherapy. Nurses may track medication efficacy and share this with the psychiatrist to adjust dosages.
- Patient-Centered Approach: The patient is at the center of the team’s efforts. By providing coordinated care across multiple disciplines, the team ensures that the patient receives comprehensive, integrated care that takes all aspects of their mental health into account.
Benefits of a Multidisciplinary Approach to Mental Health Care
- Holistic Care: By incorporating various specialists, the patient receives well-rounded care that addresses their physical, psychological, and social needs.
- Improved Treatment Outcomes: The combined knowledge and expertise of a multidisciplinary team result in more accurate diagnoses, more effective treatment plans, and better patient outcomes.
- Faster Recovery: With all professionals working together in a coordinated manner, recovery is often more efficient. This collaborative approach can prevent delays, gaps, and miscommunications that could otherwise hinder progress.
- Comprehensive Support: Patients not only receive medical and psychological care, but they also get support for social issues, life skills development, and community reintegration, all of which are essential for long-term recovery.
- Reduced Stigma: The involvement of peer support workers and the normalization of collaboration among different professionals helps reduce the stigma associated with mental health treatment. Patients feel more comfortable seeking help and more supported in their recovery journey.
Conclusion
A comprehensive mental health care pathway is a powerful tool in supporting individuals through their mental health journey, ensuring that they receive timely and effective care at every stage. From early detection and diagnosis to treatment, recovery, and long-term maintenance, the pathway integrates a wide range of services and professionals to ensure that no aspect of a patient’s mental health needs is overlooked.
The key to success in mental health care is a collaborative approach, which involves the patient, their family, and a dedicated team of mental health professionals. With the right resources and support, individuals can regain control of their mental health and achieve long-lasting well-being.
Through a comprehensive mental health care pathway, individuals can gain the tools, support, and resources necessary to achieve lasting recovery and well-being.
Frequently Asked Questions (FAQs)
What is the role of therapy in mental health recovery?
Therapy helps individuals understand their emotions, develop coping mechanisms, and address negative thought patterns. It is crucial in teaching patients how to manage stress, anxiety, and depression and improving their emotional well-being.
Can medication alone treat mental health conditions?
While medication can be effective in managing symptoms of certain mental health conditions, it is often most effective when combined with therapy and lifestyle changes. Medications alone do not address underlying psychological issues.
How long does mental health recovery take?
Recovery timelines vary widely, depending on the individual, the severity of the condition, and the treatments used. Some individuals may experience significant improvement within months, while others may require long-term care and support.
What are the signs that I need professional mental health help?
If you are experiencing persistent feelings of sadness, anxiety, or anger, difficulty concentrating, sleep disturbances, or isolation from others, it may be time to seek professional help.
Is mental health treatment covered by insurance?
Mental health treatment is increasingly covered by insurance plans, but coverage may vary. It’s essential to check with your insurer to understand the specifics of your plan, including the types of care covered.
How can family and friends support someone in mental health recovery?
Supportive relationships are essential in recovery. Family and friends can offer emotional support, encourage treatment adherence, help manage stressors, and provide a safe and understanding environment.
Can mental health conditions be prevented?
While not all mental health conditions are preventable, early intervention, stress management, and building healthy coping skills can help reduce the risk of developing severe mental health issues.

